Osteoporosis: Building Better Bones
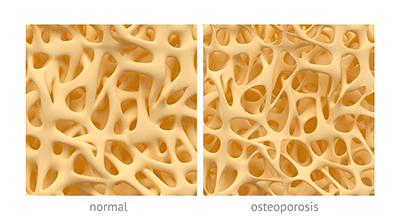
The most common condition of the bones, by far, is osteoporosis. As you likely know, osteoporosis is characterized by a decreased bone mass and deterioration of the bone tissues. You can think of your bones like a bridge over a body of water: They are both supported by a fine crosshatched matrix that keeps them strong. If there is any compromise to this structure of the bridge, it is likely to break due to stress. Thus, osteoporosis or loss of bone density is a problem because it can lead to an increased risk of fracture. The most common areas of fracture are the spine, the wrist, and—most dangerously—the hip.
Osteoporosis does not happen overnight; it has actually been termed the “silent thief” because we can lose bone mass for years with no symptoms.
Similarly, it often takes time to build bone back up with treatment. Fractures from osteoporosis are more common than heart attack, stroke, and breast cancer combined—at least one in three women and one in five men will suffer from an osteoporotic fracture during their lifetime.[1] The yearly estimated cost for the Canadian health-care system for the treatment of these fractures is roughly 2.3 billion dollars.[2] Risk factors include age over 65, low body weight, history of smoking, high alcohol intake (three or more alcoholic drinks per day for women), diabetes, and medications like steroids, sleeping pills, and some antidepressants.[3]
 Hormones and Bone Health
Hormones and Bone Health
Bone health is a great balancing act throughout life. It is dependent on two different types of cells called osteoblasts and osteoclasts—osteoblasts help build bone, while osteoclasts break it down. Before the age of about 30 years old, bone production is greater than bone loss, but you can probably guess this changes rapidly as we age.
An interesting observation is that postmenopausal women account for 80 percent of all cases of osteoporosis. The major reason that this shift happens in the body after menopause is a drop in estradiol, the most potent form of our estrogen. This hormone is important because it is thought to stimulate bone formation by osteoblasts.[4]
A similar hormone, called testosterone, can help protect bone density in men. Men are also at risk of developing osteoporosis, but they tend to do so 5 to 10 years later than women, since testosterone levels do not fall abruptly the way estrogen does in women.[5] It is estimated that osteoporosis will cause half of all women over age 50 to suffer a fracture of the hip, wrist, or vertebra due to osteoporosis.[6]
Getting the most bang for your buck when it comes to bone production is easiest before the age of 30, when bone is rapidly deposited, providing a solid foundation to protect against future fractures. Although bone develops at a slower rate after this age, it is never too late to start improving your bone health. Many complex factors can influence bone loss including genetics, low levels of activity, and hormonal changes, as discussed. Research has also identified early use of oral contraceptives as a concern for bone development. Adolescents who use hormonal birth control before they have had their menstrual cycle for three years may be stunting development of peak bone density at this age. This is because even a low dose of ethinyl estradiol, found in birth-control pills, inhibits the body’s own release of estrogen, which can change hormone levels and prevent the accrual of bone mass.[7] Malnutrition due to eating disorders is also a concern in this age group and can lead to stunted bone mass development.
 Measuring Bone Density
Measuring Bone Density
Detecting osteoporosis is the first step to prevention of fractures and proper treatment. This is done using a DXA scan (also called a bone scan), which is a special type of X-ray that can detect how dense a bone is. The way it works is like shining a light through a curtain—if lots of light ends up on the other side, then the curtain is thin. If a large amount of X-rays shine through the bone, the density is either classed as osteopenia (the beginning stages of osteoporosis) or osteoporosis. Screening generally starts at the age of 50 and should be done every five years.
Regardless of your bone density, it is still a great idea to be proactive about your bone health at any age. Here are a few key steps you can take to prevent or treat osteoporosis naturally.
Build Your Bones
Keep Moving
Several types of exercise are recommended for osteoporosis. The main form is classified as weight-bearing exercise, which is any exercise in which you are moving against the force of gravity. This type of exercise helps to build muscle, which in turn pulls on bone and stimulates growth through activation of osteoblasts. Examples of this could be walking, jogging, dancing, or stair-climbing. The recommended amount of weight-bearing exercise for treatment and prevention of bone loss is 30 minutes most days of the week. Stretching can be equally important, and it can help maintain mobility and decrease pain in those with osteoporosis.[8]
Perfect Your Balance
Balance is important when we age, to prevent falls which could lead to serious fractures if you have osteoporosis. Exercising can help build core muscles, which stabilize us and help us recover from stumbles. Tai chi is one type of exercise that has been shown to help with balance and can help slow bone loss in the lumbar spine and hip.[9] A simple trick you could try to work on your balance is standing on one leg while you are brushing your teeth at night to test your balance. Make sure you always have something nearby to steady you in case you lose your balance when challenging yourself.
 Calcium, Calcium, Calcium
Calcium, Calcium, Calcium
This mineral is used by osteoblasts to build new bone. The healthiest and safest level of calcium consumption is somewhat controversial, and it is possible to get your daily requirements through food even if you don’t eat dairy. General recommendations state that anyone under 50 years of age should consume 1,000 mg of calcium per day, and 1,200 mg for those who are over 50 years of age. There is a chance of getting too much calcium as well—anything over 2,500 mg per day can affect kidney function and deplete the body of other minerals like zinc, magnesium, and iron.
I usually assess each patient’s diet to see how much calcium they are already getting, and I suggest a low-dose supplement and dietary changes if needed.
What type of calcium should you choose? When selecting a calcium supplement, the form of calcium you choose is important, and so is the amount of elemental calcium it contains. This is the form of calcium that we actually absorb. Calcium citrate is a common form found in drugstores that does not usually cause digestive upset, but it does not contain much elemental calcium. Calcium carbonate is another form you may see that has more elemental calcium than calcium citrate, but it may cause gas or constipation. Calcium phosphate is less common, but is available in some products; it has as much elemental calcium as calcium carbonate, but is better absorbed and does not cause any digestive upset. It is the most expensive form of calcium. It is important not to take any calcium supplement at the same meal as medications, as the calcium may decrease the absorption of many medications. Taking calcium with iron will also decrease absorption.
 The Sunshine Vitamin
The Sunshine Vitamin
Vitamin D is a close second to calcium when it comes to importance for bone health. Vitamin D is actually converted to a hormone called calcitriol, which helps us absorb calcium from our diet or supplements and may stimulate bone growth. Talk to your doctor about measuring your vitamin D levels and finding out what dosage is best for you.
Vitamin K
We are now discovering that this fat-soluble vitamin has many hats, playing a role in blood clotting, cellular growth, and even bone health. Some research has shown that vitamin K can help stimulate bone growth and prevent fractures in subjects with osteoporosis. Just like vitamin D, this vitamin may help increase our body’s absorption of calcium and provide more building blocks for our bones.[10] Increase your intake of dark leafy greens as a rich source of vitamin K.
Conclusion
If you have been diagnosed with low bone density or are looking to help support your bone health at any point, booking an appointment with a naturopathic doctor is a great way to get started in the right direction.
 Dr. Sarah Penney, ND, MSc
Dr. Sarah Penney, ND, MSc
A graduate of the CCNM in Toronto, Sarah has a special interest in women’s health, fertility, digestive concerns, pain management, and chronic disease.
completenaturalhealth.ca
References
- Gulsahi, A. “Osteoporosis and jawbones in women.” Journal of International Society of Preventive & Community Dentistry, Vol. 5, No. 4 (2015): 263–267.
- Tarride, J.E., et al. “The burden of illness of osteoporosis in Canadian men.” Journal of Bone and Mineral Research, Vol. 27, No. 8 (2012): 1830–1838.
- Schürer, C., et al. “Fracture risk and risk factors for osteoporosis.” Deutsches Arzteblatt International, Vol. 112, No. 21–22 (2015): 365–371.
- Syed, F., and S. Khosla. “Mechanisms of sex steroid effects on bone.” Biochemical and Biophysical Research Communications, Vol. 328, No. 3 (2005): 688–696.
- Falahati-nini, A., et al. “Relative contributions of testosterone and estrogen in regulating bone resorption and formation in normal elderly men.” The Journal of Clinical Investigation, Vol. 106, No. 12 (2000): 1553–1560.
- Crandall, C.J., et al. “Osteoporosis screening in postmenopausal women 50 to 64 years old: Comparison of US Preventive Services Task Force Strategy and two traditional strategies in the Women’s Health Initiative.” Journal of Bone and Mineral Research, Vol. 29, No. 7 (2014): 1661–1666.
- Scholes, D., et al. “Oral contraceptive use and bone density in adolescent and young adult women.” Contraception, Vol. 81, No. 1 (2010): 35–40.
- Shanb, A.A., and E.F. Youssef. “The impact of adding weight-bearing exercise versus nonweight bearing programs to the medical treatment of elderly patients with osteoporosis.” Journal of Family and Community Medicine, Vol. 21, No. 3 (2014): 176–181.
- Zou, L., et al. “The effect of taichi practice on attenuating bone mineral density loss: A systematic review and meta-analysis of randomized controlled trials.” International Journal of Environmental Research and Public Health, Vol. 14, No. 9 (2017): E1000.
- Weber, P. “Vitamin K and bone health.” Nutrition, Vol. 17, No. 10 (2001): 880–887.

 Stores
Stores