The Development of Food Sensitivities
True and False Sensitivities and What to Do About Them
 A hundred years ago, the idea of being “sensitive” to a food would have been absurd. Even just a decade ago, the terms “gluten-free” or “dairy allergy” were uncommon, and most people judged without knowing what it meant or why it was important. Today, most schools are nut-free facilities, and laws have been passed to ensure proper labeling of all ingredients in a product. Still, many families struggle with the idea of keeping certain foods off the dinner table, and if you are someone with a food sensitivity, you know how stressful it can be to attend any social gathering. What has triggered this development in sensitivities to food? Has our food changed so drastically that we no longer recognize it, or have our bodies become more sensitive? Perhaps the answer is a combination of both but, given the human genome has been nearly identical for last 2000 years, it is unlikely to be a gene mutation.
A hundred years ago, the idea of being “sensitive” to a food would have been absurd. Even just a decade ago, the terms “gluten-free” or “dairy allergy” were uncommon, and most people judged without knowing what it meant or why it was important. Today, most schools are nut-free facilities, and laws have been passed to ensure proper labeling of all ingredients in a product. Still, many families struggle with the idea of keeping certain foods off the dinner table, and if you are someone with a food sensitivity, you know how stressful it can be to attend any social gathering. What has triggered this development in sensitivities to food? Has our food changed so drastically that we no longer recognize it, or have our bodies become more sensitive? Perhaps the answer is a combination of both but, given the human genome has been nearly identical for last 2000 years, it is unlikely to be a gene mutation.
Countless books have been written showcasing different perspectives on the ideal way to support and maintain a healthy digestive tract. Diets have been developed for specific diseases, and while some avoid a food allergen forever, others think that avoidance worsens the immune response. So how do we decide the best way to manage a food sensitivity and to determine the difference between true and false reactions? Let’s start by looking at how the digestive system and immune system are interrelated.
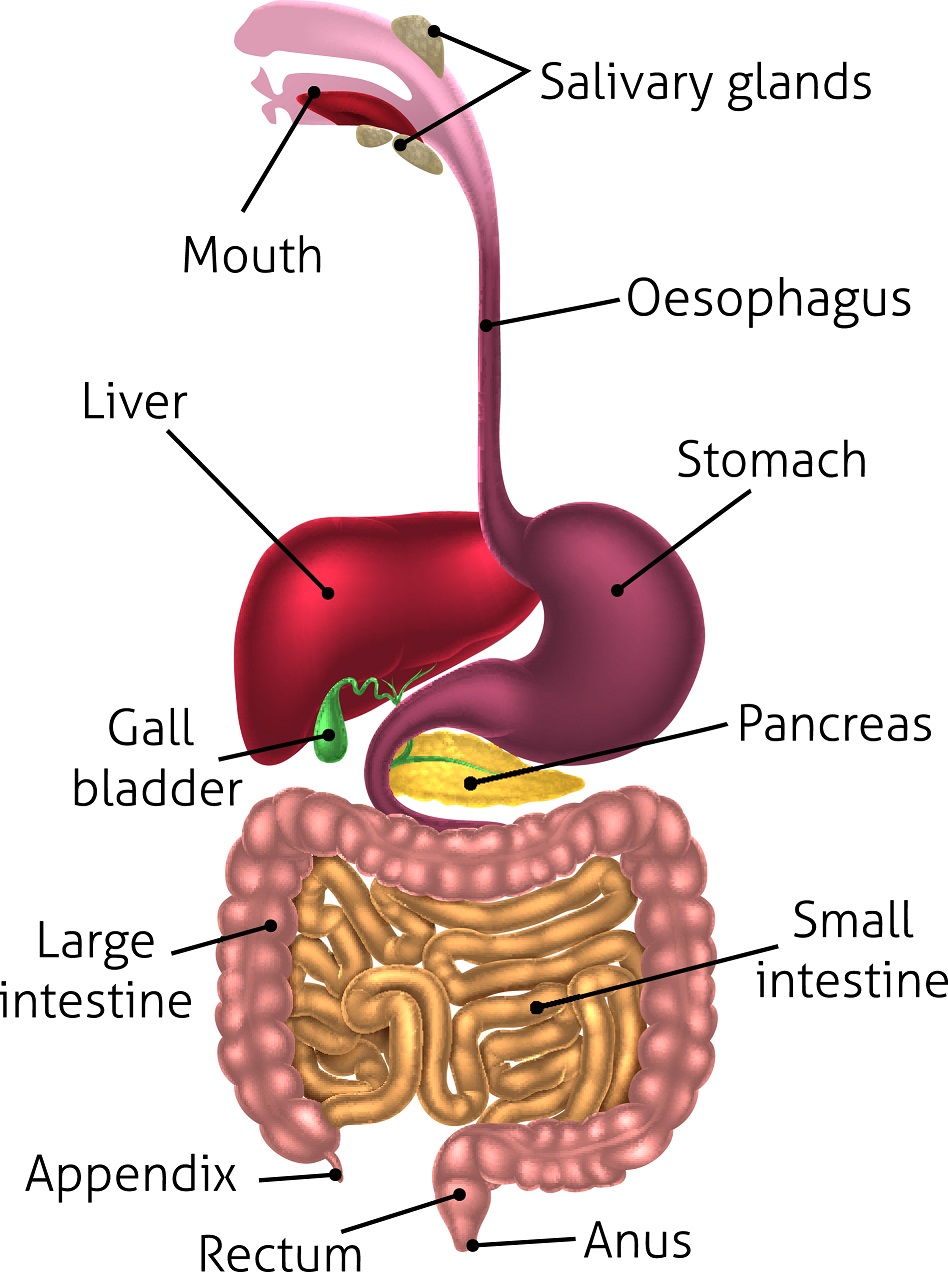 The gastrointestinal tract has an
The gastrointestinal tract has an
intricate anatomy that requires
specific conditions to be met for
proper digestion and absorption
of nutrients. Food entering the
stomach must be broken down
to the smallest particle in order
to be absorbed through the very
tight gaps between cells of the
stomach lining and into the
bloodstream.[1]
This first step can be
complicated by inadequate
production of digestive enzymes, insufficient stomach acid, and
rapid transit through the stomach
with overactive muscles. In the
case of a highly stressed person
who eats on the go and doesn’t
thoroughly chew their food, large
pieces of food require more
stomach acid and more digestive
enzyme activity to properly break
them down. Insufficient stomach
acid and enzyme levels will
prevent large pieces of food from
being digested, causing these pieces to remain in the digestive tract and attract water to the area, resulting in bloating. If there is damage to the stomach lining from antibiotic use, drug use, alcohol abuse, stress, or infection, the gaps between cells of the intestine become wider and allow these large pieces to enter right into the bloodstream.
 Now, let’s consider the immune response to this. As the immune system is used to seeing the smallest particles of food in the blood, large pieces are extremely foreign and an immediate attack ensues. Immune cells are produced to fight those specific foods, and travel around the entire body looking for other foreign particles to attack. This can cause inflammation in muscles, joints, and skin; decrease focus and concentration; and eat away at your energy, leaving you feeling sluggish. As for the remaining food in the digestive tract that is not absorbed, water and bacteria rush in to ferment and create symptoms of bloating and gas. Over time, the repeated entrance of improperly digested foods creates a proportionately larger immune response, which can result in eczema, acne, headaches, weight gain, fatigue, joint pain, and even depression.
Now, let’s consider the immune response to this. As the immune system is used to seeing the smallest particles of food in the blood, large pieces are extremely foreign and an immediate attack ensues. Immune cells are produced to fight those specific foods, and travel around the entire body looking for other foreign particles to attack. This can cause inflammation in muscles, joints, and skin; decrease focus and concentration; and eat away at your energy, leaving you feeling sluggish. As for the remaining food in the digestive tract that is not absorbed, water and bacteria rush in to ferment and create symptoms of bloating and gas. Over time, the repeated entrance of improperly digested foods creates a proportionately larger immune response, which can result in eczema, acne, headaches, weight gain, fatigue, joint pain, and even depression.
Because the immune cells are made to identify a specific part of a food, for example the gluten protein, a seeming “gluten sensitivity” develops. Now, celiac disease is a completely different story, because immune cells specific to gluten are delivered genetically, and these individuals will never be able to tolerate gluten.[2] The good news for the rest of us is that simply removing gluten for a few weeks and adding in a few healing nutrients can allow the digestive lining to seal those tight junctions. Proper eating habits—like sitting down to eat a meal, chewing thoroughly, and not wolfing down food—allow the body’s natural production of digestive enzymes and stomach acid to increase. With some time and effort, it is possible to overcome a food sensitivity and get back to enjoying foods again.
So now that we have outlined the basic idea of a leaky gut picture and discussed how gaps within the stomach lining can create symptoms of food sensitivities, let’s also consider the difference between a true and a false food sensitivity.
False sensitivities occur because of inflammation in the gastrointestinal tract from:
-
Inadequate stomach acid production;
-
Insufficient digestive enzyme production;
-
Overconsumption of processed and inflammatory foods; or
-
Damage to the digestive tract from external sources such as drugs, alcohol, antibiotics, etc.
True sensitivities occur when these other factors have all been considered, the gut has been healed, and yet the individual still experiences a certain set of symptoms after consuming the food.
So how will we know if someone has a true or a false sensitivity? Well, as health-care practitioners, we must determine the best course of treatment based on our individual patient and the information we gather in our assessment. Every practitioner manages gut health slightly differently, but since digestive health is the basic function for absorbing all our nutrients, it absolutely must be considered.
 Food Sensitivity
Food Sensitivity
Testing: This test is
often done through naturopathic doctors,
and involves taking a sample of blood and sending it off to a specialized lab. The
blood is tested against
a series of foods and is reported back with a number and colour
scale showing the
severity of the reaction. The accuracy of the test has been questioned over the years, but generally people find it easier to remove a selected list of foods from their diet, and almost always feel significantly better upon avoidance.
Elimination or Hypoallergenic Diet: This is a diet that involves avoidance of the most common food sensitivities for at least six weeks. This can be done for people who do not want to do the food sensitivity test, or can be modified based on the results of the test. The beauty of this diet is that gut healing begins and continues over the course of the six weeks of avoidance. Within one week, bloating and gas can noticeably decline, energy levels increase, and sleep depth improve. The most important, and often difficult, part of this elimination is the reintroduction at the end, which involves adding one food back at a time and monitoring the health concerns and associated symptoms. At the end of the process, the individual comes away with a list of their true sensitivities, the knowledge of the exact symptoms each food causes them, and a healed gut with proper digestive function.
As mentioned earlier, the management of a “leaky gut” can be different for each practitioner, but some of the most highly recommended products include:
Betaine Hydrochloride: Taken along with the elimination diet, to increase the production of stomach acid and to reactivate the natural signalling to produce stomach acid naturally.
Digestive Enzymes: Taken with meals over the course of the avoidance phase, to encourage the breakdown of foods and again reset the natural signalling to produce digestive enzymes. Most people notice decreases in bloating and gas within a few days of starting a digestive enzyme.
Glutamine: This amino acid is food for the cells of the intestine and helps them to rebuild. I have had mixed reviews on this, and many patients do not always feel better adding glutamine to their routine.
EGCG (Green Tea Extract): This powerful antioxidant is not always used for digestive health, but has a role in boosting metabolism and regulating the balance of good and bad bacteria in the gut. While it functions differently than a probiotic and should not be used as a substitute, it is a suitable adjunct for rebuilding a healthy balance in the gut.
 Probiotics: As
Probiotics: As
mentioned above,
adding good bacteria
is essential in re-establishing the balance between
good and bad bacteria
in the gut. Because so much of the immune
system lives within our gastrointestinal tract
and in the bacteria
that reside there, it is important to keep an
adequate number of
good guys.
Magnesium: A micromineral with multiple uses and actions all over the body. In this specific context, we are considering magnesium for its benefit on the digestive tract and re-establishing gut motility. Magnesium acts similarly to an osmotic laxative, and when consumed in large amounts, draws water into the intestines and results in loose bowel movements. The goal in gut healing is not to create diarrhea, but instead to ensure regular motility and prevent constipation.
Of course, taking all these products can be overwhelming for a patient and often not necessary. Find the best combination of products for each patient and in the right sequence, and ensure that health is maintained and the development of new sensitivities is avoided.
References
- Hagen, S., et al. “Inflammation causes important changes in stomach tight junction structure and function.” The FASEB Journal, Vol. 26, No. 1 Supplement (2012): 1156.4-1156.4.
- Ciccocioppo, R., et al. “The immune recognition of gluten in coeliac disease.” Clinical & Experimental Immunology, Vol. 140, No. 3 (2005): 408–413.
 Dr. Krysten DeSouza, ND
Dr. Krysten DeSouza, ND
She strives to share her knowledge and experience with patients
to help them discover more about their health and find relief
from their ailments.
www.desouzanaturopathic.com

 Stores
Stores